The following article was taken from http://www.koffeemag.com/ : This week in Black History, Koffee takes a look through the lens of 6 women, who have impacted our communities, made a difference in the lives around them, and contribute countless hours of volunteering without reward or recognition. We honor Philippa Schuyler, Sissieretta Jones, Dr. Adele D. Allen, Scharmaine Lawson-Baker, Shoshana Johnson, and Pastor Je’Nise Goss.
Scharmaine Lawson-Baker contributed her story: "Holistic Care in the Eye of the Storm," to the book To the Rescue:Healthcare Workers at the Scenes of Disasters.
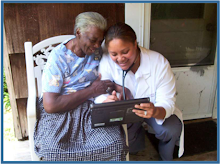
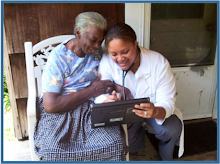
f it weren’t for Scharmaine Lawson-Baker, some of the elderly, poor and disabled in New Orleans would receive any medical care. She’s willing to make house calls, whether it is to a FEMA trailer, the projects, group homes or assisted living facilities.
Lawson-Baker, DNP, FNP-BC, a nurse practitioner, initiated Advanced Clinical Consultants in 2005 with a mission to provide a house call to every senior or disabled person in New Orleans who is unable to visit their regular primary care physician. In addition, she runs a non-profit clinic two days a week.
Lawson-Baker also created a non-profit, Geriatric Initiatives, that is staffed with volunteers to assist patients/clients with obtaining resources to maintain their housing/residence, address their mental and behavioral health concerns, purchase medications, obtain medical equipment, transit services, scheduling of medical appointments, obtaining food stamps, among other services. Her philosophy is that no one, especially and 85-year-old woman surviving off of $300 per month in Social Security Income should have to decide whether to purchase sanitary needs or buy medication.
Several months after she opened her business, Hurricane Katrina hit, making her services more vital than ever. She visited crumbling houses on abandoned, debris-strewn streets.
“I love everything I do. I enjoy meeting a need. A lot of my patients are in the 9th Ward and lack heath care. Where care is available, there is a long waiting list to see a health care provider. If I didn’t see them, they otherwise probably wouldn’t get care. This is my passion,” says Lawson-Baker.
Today she remains the lone nurse practitioner making house calls, but she one day hopes to be able to add someone part-time assistance. Growing her business is a challenge as her primary source of income comes from Medicaid and Medicare. But, Lawson-Baker, 42, doesn’t do what she does because she’s motivated by money. “I like making a difference.”